CASE REPORT | https://doi.org/10.5005/jp-journals-10083-0931 |
Differential Diagnosis of a Multilocular Radiolucency of the Mandible: A Case Report
1,2Department of Oral Medicine and Radiology, Indira Gandhi Institute of Dental Sciences, Sri Balaji Vidyapeeth, Puducherry, India
Corresponding Author: Yazhini Malairaj, Department of Oral Medicine and Radiology, Indira Gandhi Institute of Dental Sciences, Sri Balaji Vidyapeeth, Puducherry, India, Phone: +91 9487138847, e-mail: yazhini210894@gmail.com
How to cite this article Malairaj Y, Reddy J. Differential Diagnosis of a Multilocular Radiolucency of the Mandible: A Case Report. J Sci Dent 2020;10(2):46–48.
Source of support: Nil
Conflict of interest: None
ABSTRACT
Odontogenic keratocyst is classified under developmental cyst which develops from cell rest of dental lamina. It has no specific predilection for age and can occur from infancy to old age, however with a slight predilection for males. The mandibular posterior region is most commonly affected. The cyst has high chances of recurrence. One of the most important radiographic features is that the cyst tends to expand antero-posteriorly within the medullary cavity of the bone without causing bony expansion. A case with odontogenic keratocyst of the left posterior mandible is discussed with clinical and radiographic findings. Clinical examination revealed buccal lymphadenitis with obliteration and tenderness over the left mandibular buccal vestibule. Radiographic examination such as intraoral periapical (IOPA) radiograph and orthopantomogram revealed a multilocular lesion with mixed densities involving the apices of the left mandibular posterior teeth. The corresponding third molar was impacted and the inferior alveolar nerve canal was displaced inferiorly. There was no bony expansion evident on the occlusal radiograph. The features were suggestive of odontogenic keratocyst.
Keywords: Ameloblastoma, Dentigerous cyst, Odontogenic keratocyst, Odontogenic myxoma..
INTRODUCTION
Odontogenic keratocyst is a developmental odontogenic cyst1 whose origin is from cell rest of dental lamina.1,2 It causes local destruction of tissues, has high chances of recurrence, and is associated with nevoid basal cell carcinoma syndrome.3 Odontogenic keratocyst can rarely transform into ameloblastoma and primary intra-osseous carcinoma.4 Due to its neoplastic potential, odontogenic keratocyst is considered as a benign neoplastic cyst. In 2005, the WHO reclassified this lesion as a tumor—“keratocystic odontogenic tumor.”5 Next to the radicular cyst and dentigerous cyst, odontogenic keratocyst is the most common type of odontogenic cyst.6 It accounts for about 3% to 11% of all odontogenic cysts.1 The odontogenic keratocyst most often occurs in the second and third decades of life with slight male predilection.6 The mandibular posterior region is most commonly affected.7
CASE DESCRIPTION
A 50-year-old female reported to the Department of Oral Medicine and Radiology, Indira Gandhi Institute of Dental Sciences, Sri Balaji Vidyapeeth, Puducherry with a chief complaint of pain over the left lower back teeth region for past 2 weeks. The pain was sudden in onset, pricking type, intermittent in nature, mild in intensity, aggravates while chewing food, and relieves on taking medications. Medical history was unremarkable. The patient gave no history of hazardous habits. The patient’s vital signs were within normal limits. On local examination, a single oval-shaped buccal lymph node was present over the left side lower third of face measuring 1 × 1.5 cm, mobile, firm in consistency, and with tenderness (Fig. 1). Intraoral examination revealed an obliterated left buccal vestibule which was tender on palpation (Fig. 2).
Radiographic investigations included intraoral periapical radiograph, left mandibular occlusal and orthopantomogram. IOPA in relation to 35, 36 and 37 presented with a well-defined radiolucency with scalloped border involving the apical portion of the teeth. The internal structure showed mixed densities (haziness present with respect to 37 region). A loss in continuity of lamina dura was evident with an altered trabecular pattern. Crestal bone loss was seen with respect to 35 and furcation bone loss was evident with respect to 36. Supra-erupted 36 and impacted 38 were evident (Fig. 3). The mandibular left occlusal radiograph revealed no cortical bone expansion (Fig. 4).
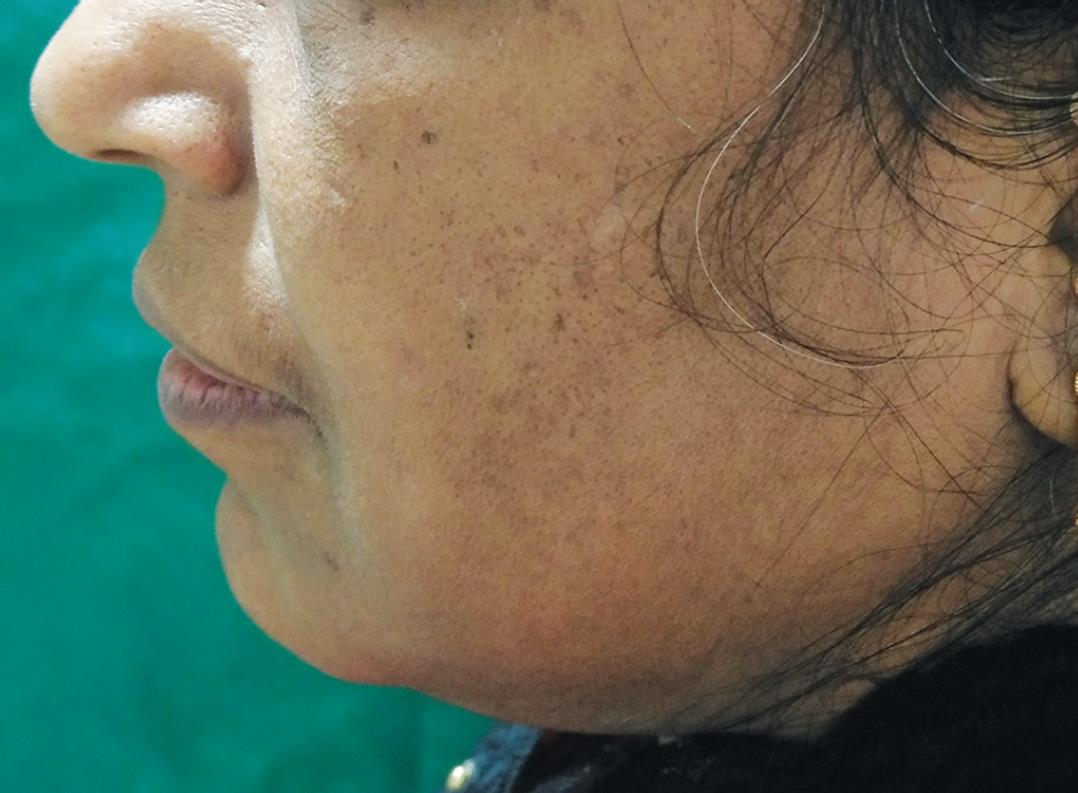
Fig. 1: Left buccal lymphadenitis

Fig. 2: Obliteration of the left side of mandibular buccal vestibule

Fig. 3: Intraoral periapical radiograph of 35, 36 and 37

Fig. 4: Occlusal radiograph

Fig. 5: Orthopantomogram showing multilocular lesion over the left-side body of the mandible and ascending ramus
Orthopantomogram presented with a unilateral multilocular radiolucency on the left posterior mandible involving the ramus measuring 4 × 2 cm with scalloped borders. The internal structure was radiolucent with the areas of haziness. The anterior radiolucency showed curved septa, and the posterior radiolucency showed fine horizontal septa (wispy septa). The inferior alveolar nerve canal was displaced inferiorly. An impacted third molar (38) was evident in the region. The lesion was extending anteroposteriorly with no cortical bone expansion (Fig. 5).
The radiographic diagnosis was given as odontogenic keratocyst due to the presence of the following features: posterior body of mandible was involved, invades along the internal aspect of the mandible with no cortical bone expansion, and scalloped borders; epicenter is located superior to the inferior alveolar nerve canal.8 The differential diagnosis of odontogenic myxoma due to the presence of straight thin wispy septa is one of the classical radiographic features.9 The other differential diagnosis includes dentigerous cyst (associated with the crown of unerupted tooth, has scalloped borders, and the inferior alveolar nerve canal is displaced inferiorly), ameloblastoma (multilocular scalloped lesion but has a greater proclivity to expand), and simple bone cyst (has scalloped margin and minimal bone expansion).8
DISCUSSION
The odontogenic keratocyst arises from the remnants of dental lamina, and its biologic behavior is similar to benign neoplasm.3 There is slight male predilection and the mandible is involved in 60% to 80% of cases. The odontogenic keratocyst tends to grow in the antero-posterior region within the medullary cavity of the bone without causing bony expansion. An unerupted tooth is involved in 25% to 40% cases. The resorption of the roots of the tooth is less common.1 It is locally aggressive and has a high recurrence rate.3 The management of odontogenic keratocyst depends on the site and extent of the lesion.10 The surgical treatment may vary and can include resection, curettage, or marsupialization to reduce the size of large lesions before surgical excision.8
The case discussed has findings supportive of the odontogenic keratocyst such as mandible is involved, associated with an unerupted tooth and the lesion is found anteroposteriorly within the medullary cavity of bone with no cortical expansion. The radiographic differential diagnosis includes odontogenic myxoma, dentigerous cyst, ameloblastoma, and simple bone cyst. The odontogenic myxoma accounts for about 3% to 6% of odontogenic tumors. The presence of straight thin septa is considered to be the important characteristic feature of odontogenic myxoma. It causes cortical bone expansion at the later stages.9 The dentigerous cyst accounts for about 20% of all jaw cyst and is most commonly associated with impacted mandibular third molar. It is a slow-growing cyst that often expands the cortical bone.11,12 Ameloblastoma accounts for about 9% of all odontogenic tumors. It is a multilocular lesion and occurs most commonly in the molar-ascending ramus region. Buccal and lingual cortical bone expansion is often noted.13 A simple bone cyst is not a true cyst and is more common in the mandible. It has an oval or scalloped border. The expansion of bone is more common in larger lesions.14
CONCLUSION
The case presented to be a unilateral multilocular lesion with mixed radiodensities and extending anteroposteriorly with no cortical bone expansion. Though the definite diagnosis of odontogenic keratocyst cannot be provided only with clinical and radiographic findings, they provide essential knowledge about the distinctive features needed for diagnosis and treatment planning. They also help for evaluating the extent of the lesions and the relationships with adjacent structures.15 Based on the characteristic radiographic appearance, a radiographic diagnosis of odontogenic keratocyst was made.
DECLARATION OF PATIENT CONSENT
The authors certify that they have obtained all appropriate patient consents. The patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
REFERENCES
1. Neville BW, Damm DD, Allen CM, et al. Oral and maxillofacial pathology. Elsevier Health Sciences; 2013.
2. Sekhar MC, Thabusum DA, Charitha M, Chandrasekhar G, Shalini M. A review of the odontogenic keratocyst and report of a case. Journal of Advances in Medicine and Medical Research 2019. 1–7. DOI: 10.9734/jammr/2019/v29i830107.
3. Rajendran R, Sivapathasundharam B. Shafer’s Textbook Of Oral Pathology. India: Elsevier; 2012.
4. Nair KK, Lingappa A, Rangaiah P, Vittobarao PG. Keratocystic odontogenic tumor: a case report and review of literature. Indian Acad Oral Med Radiol 2015;27(2):253. DOI: 10.4103/0972-1363.170148.
5. Bohra A, Udawat V, Bhemappa A, Arya S. Keratocystic odontogenic tumor of mandible. Med J DY Patil Vidyapeeth 2016;9(3):403. DOI: 10.4103/0975-2870.182524.
6. Karandikar S, Nilesh K, Dadhich A. Large odontogenic keratocyst of mandible. A case report. J Indian Dent Assoc 2011;7:822–824.
7. Kambalimath DH, Kambalimath HV, Agrawal SM, Singh M, Jain N, Anurag B, et al. Prevalence and distribution of odontogenic cyst in indian population: a 10 year retrospective study. J Maxillofac Oral Surg 2014;13(1):10–15. DOI: 10.1007/s12663-012-0450-y.
8. White SC, Pharoah MJ. Oral Radiology: Principles and Interpretation. Elsevier Health Sciences; 2014. DOI: 10.1016/j.oooo.2014.06.001.
9. Buch SA, Babu SG, Rao K, Rao S, Castelino RL. A large and rapidly expanding odontogenic myxoma of the mandible. J Oral Maxillofac Radiol 2017;5(1):22. DOI: 10.4103/jomr.jomr_49_16.
10. Belgal PG, Pathak B, Shastry L. Updates in the surgical management of odontogenic keratocyst. J Adv Clin Res Insights 2019;6(4):116–118. DOI: 10.15713/ins.jcri.273.
11. Robinson RA. Diagnosing the most common odontogenic cystic and osseous lesions of the jaws for the practicing pathologist. Modern Pathology 2017;30(1):S96–S103. DOI: 10.1038/modpathol.2016.191.
12. Zerrin E, Husniye DK, Peruze C. Dentigerous cysts of the jaws: clinical and radiological findings of 18 cases. J Oral Maxillofac Radiol 2014;2(3):77. DOI: 10.4103/2321-3841.144673.
13. More C, Tailor M, Patel HJ, Asrani M, Thakkar K, Adalja C. Radiographic analysis of ameloblastoma: a retrospective study. Indian J Dent Res 2012;23(5):698. DOI: 10.4103/0970-9290.107436.
14. Sudha SG, Thomas S, Nair VV. Simple bone cyst presenting as an incidental finding in pretreatment orthodontic radiograph: a case report. J Indian Acad Oral Med Radiol 2017;29(1):53. DOI: 10.4103/jiaomr.JIAOMR_128_16.
15. Borghesi A, Nardi C, Giannitto C, Tironi A, Maroldi R, Di Bartolomeo F, et al. Odontogenic keratocyst: imaging features of a benign lesion with an aggressive behaviour. Insights Imaging 2018;9(5):883–897. DOI: 10.1007/s13244-018-0644-z.
________________________
© The Author(s). 2020 Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/), which permits unrestricted use, distribution, and non-commercial reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.